Radio waves change cell DNA
 Radio waves can tune up bacteria to become life-saving medicines.
Radio waves can tune up bacteria to become life-saving medicines.
Scientists from Australia and the United States have found a new way to alter the DNA of bacterial cells - a process used to make many vital medicines including insulin - much more efficiently than standard industry techniques.
Instead of opening bacteria cell walls with harsh chemicals or high temperatures to insert DNA, the team used high-frequency radio waves, a much gentler approach that led to many more of the cells taking on the DNA and surviving.
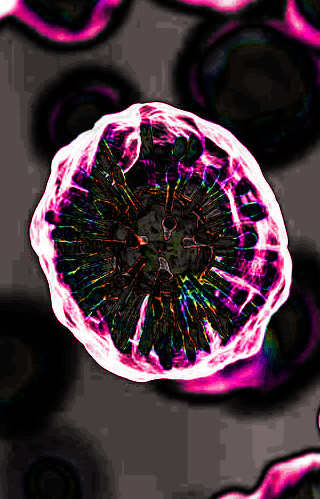
The study, led by RMIT University in collaboration with other Australian universities and WaveCyte Biotechnologies in the US, used radio waves at the 18 gigahertz frequency to temporarily ‘open the gates’ in E. coli bacterial cell walls long enough for genetic material to be inserted.
The cells then closed and continued healthy function.
Radio frequencies can be used to carry everything from mobile phone and satellite data to the energy needed to manipulate bacterial cells in a lab.
Earlier joint work with the Australian Centre for Electromagnetic Bioeffects Research demonstrated how high-frequency electromagnetic energy temporarily makes bacterial cells more permeable.
This latest study published in the high-impact journal Nano Letters takes that work a step further by showing the method can be used to safely deliver DNA.
The team’s results showed the process to be highly efficient: 91 per cent of the E. coli cells took on the new DNA after exposure to 18GHz radio waves for three minutes.
Using the current industry standard for inserting DNA, known as ‘heat shock’, only 77 per cent of the cells take on the DNA and many of those die soon after from the heat exposure.
Gentler laser pulse techniques exist but less than 30 per cent of the cells take on the new DNA in that process.
Lead author, RMIT Distinguished Professor Elena Ivanova, said their approach trumped both by being both highly efficient and gentle.
“Our novel, cost-effective method is shown to be highly efficient, but also gentler on the cells as no harsh chemicals or high temperatures are used in this process,” said Ivanova, from the School of Science.
“As a result, the cell survival rate was higher than other techniques.”
The team’s research has also shown this process works in eukaryotic cells – the type we share with animals, fungi and plants, including PC 12 cell line models commonly used in neuroscience research.
“Our focus now is on translating these findings,” Ivanova said.
“We have only scratched the surface of the wide range of drug delivery applications this approach could have in microbiome therapeutics and synthetic biology.”
RMIT has applied for intellectual property protection for the technique jointly with WaveCyte Biotechnologies, a US company specialising in developing cell and gene therapy technologies.
More details are accessible here.








 Print
Print